If your child has been diagnosed with MPS1 or is currently awaiting testing, we are here for you.
Mucopolysaccharidosis Type 1 (MPS1), is a rare, severe, progressive genetic disorder that falls under the category of lysosomal storage diseases. These disorders are characterized by the body’s inability to properly break down and dispose of specific complex molecules, leading to their accumulation within cells and various organs. In the case of MPS1, there is a deficiency of an enzyme called alpha-L-iduronidase. This enzyme is essential for breaking down certain complex carbohydrates called glycosaminoglycans (GAGs) in the body.
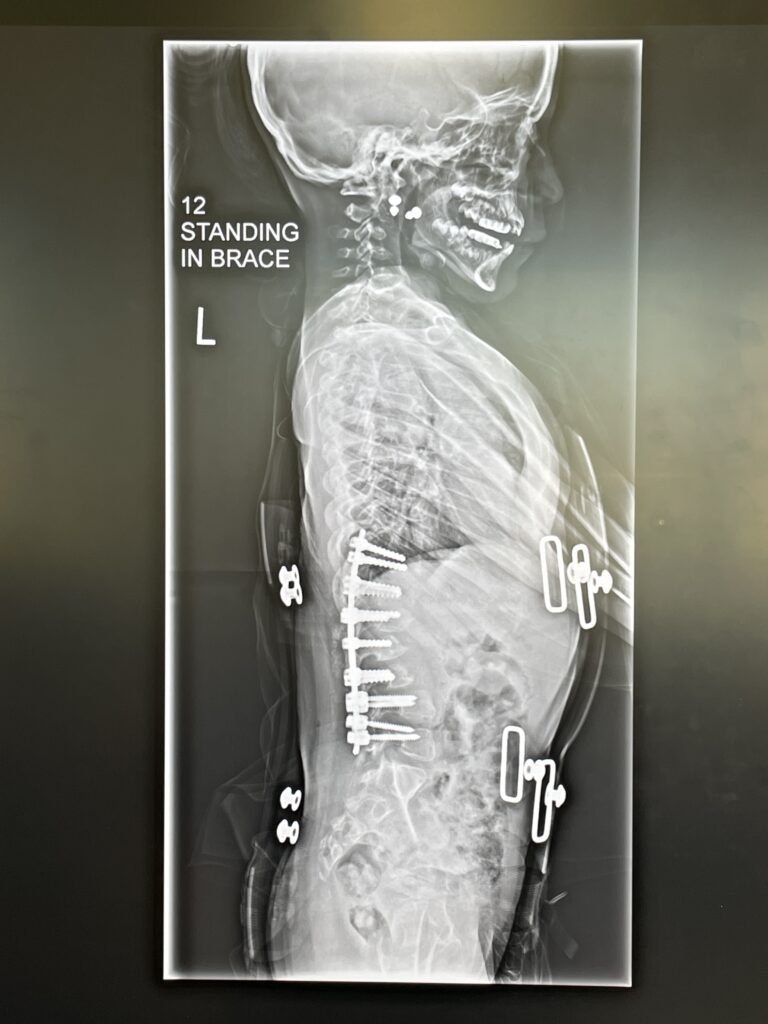
Due to the deficiency of alpha-L-iduronidase, GAGs accumulate within various tissues and organs of the body, leading to a wide range of symptoms that can affect multiple systems, including:
Hurler syndrome, Hurler-Scheie syndrome, or Scheie syndrome, depending on the severity of the condition.
The severity of the condition can vary widely, with Hurler syndrome being the most severe form and Scheie syndrome being the mildest.
There is no cure for MPS1, but treatment options may include enzyme replacement therapy (ERT) to replace the missing enzyme, bone marrow transplantation (especially for severe cases), and various supportive therapies to manage symptoms and improve the quality of life for affected individuals.
Learn more about the symptoms, how to get diagnosed, prognosis, current research, and more below:
MPS1 is a complex disorder with a wide range of symptoms. Comprehensive care often requires a multidisciplinary medical approach.

The prevalence of MPS1 can vary by subtype:
Keep in mind that these prevalence estimates can vary based on geographic location and population demographics. Advances in genetic testing and increased awareness of rare diseases may lead to more accurate diagnosis and reporting of these conditions over time.
Diagnosing MPS1, particularly Hurler syndrome, typically involves a combination of clinical evaluation, medical history, and various diagnostic tests. Here’s an overview of the diagnostic process:
If your child has been diagnosed with MPS1 or is currently awaiting testing, we are here for you. This brief MPS1 guide walks you through the initial questions most families have about MPS1, including what to do next. This introductory information is intended to help you be proactive in caring for your child and giving them the best quality of life.